Our digestive system and brain communicate closely through what researchers call the gut-brain axis. This two-way network links the central nervous system to our gastrointestinal tract via nerves, hormones, immune signals and metabolic pathways. In fact, the gut has been called a “second brain” because gut microbes produce many of the same neurotransmitters that regulate mood – including serotonin, dopamine and GABA. Roughly 90–95% of the body’s serotonin originates in the gut. When we are stressed or anxious, brain signals travel down the vagus nerve and influence digestion; conversely, gut imbalances (from diet, inflammation or microbes) send signals up that can affect stress and mood. Growing scientific evidence shows that what we eat – through its effects on gut bacteria and gut lining – can meaningfully influence our mood, stress levels, and risk for anxiety or depression. This article reviews the research and explains practical ways to nourish your gut for better mental health.
The Gut-Brain Axis: How Gut and Brain Communicate
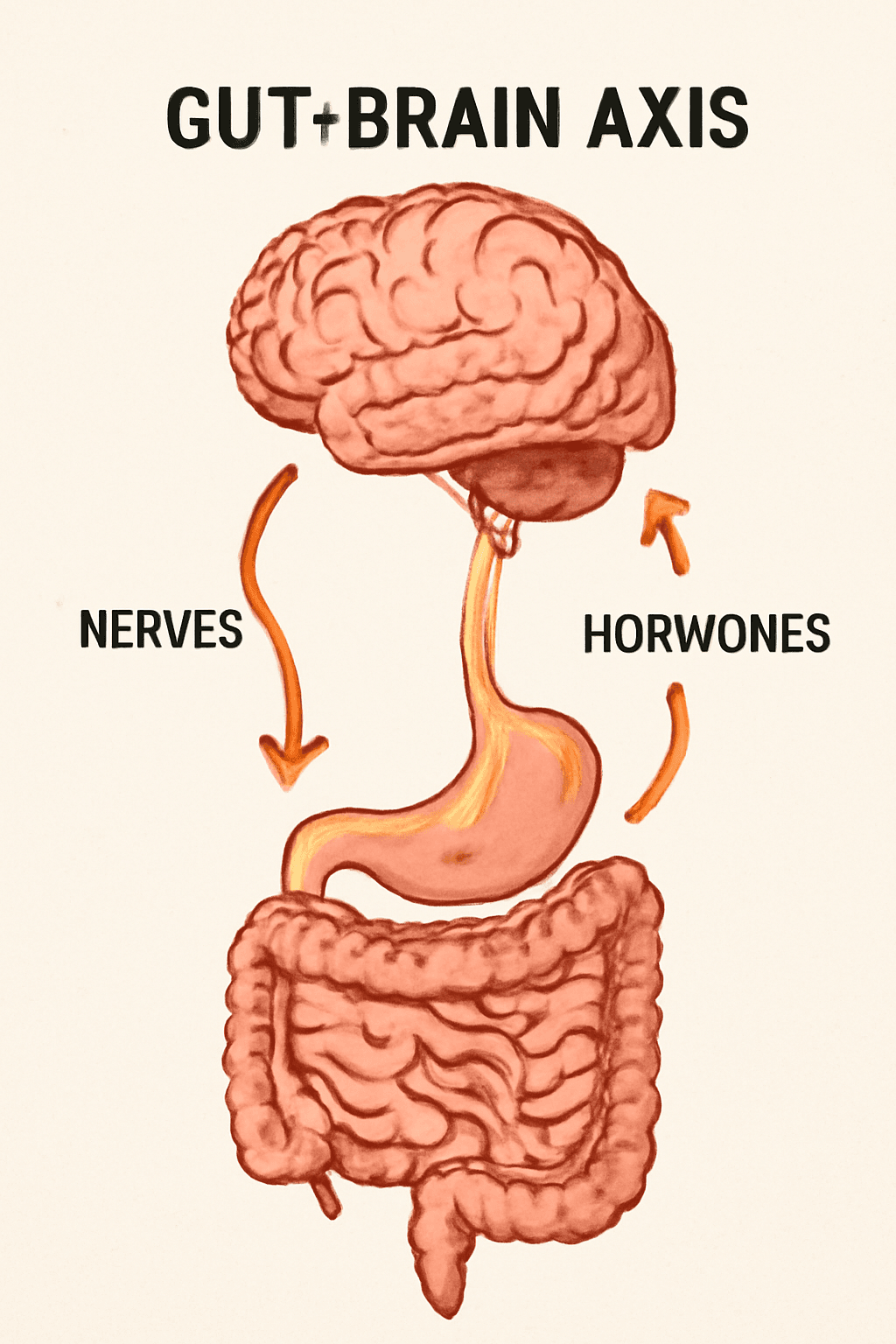
The gut-brain axis is a complex network of connections. Nervous pathways (the vagus nerve and enteric nervous system) carry signals directly between the gut and brain. Gut microbes also influence the endocrine system (hormones like cortisol, the “stress hormone”) and the immune system (cytokines and inflammation). For example, intestinal bacteria help regulate the hypothalamic-pituitary-adrenal (HPA) axis, which governs stress responses. When gut microbes are balanced, they produce short-chain fatty acids (SCFAs) and neurotransmitters that calm inflammation and maintain a healthy gut lining. But when the microbiome is disturbed (dysbiosis), it can trigger systemic inflammation and “leaky gut,” allowing bacterial byproducts (like lipopolysaccharide, LPS) into the bloodstream. These inflammatory signals reach the brain and can alter neurotransmitter levels and mood.
In short, gut bacteria influence neurochemistry and immunity. They produce SCFAs that help regulate brain-cell function, and they contribute to serotonin synthesis (the gut alone supplies most of the body’s serotonin). Disruptions of this axis – for example from chronic stress or a poor diet – have been linked to anxiety and depression in both animals and humans. Conversely, intentional changes to diet or probiotics can improve gut health and produce measurable mood benefits.
Gut Microbes, Neurotransmitters and Inflammation
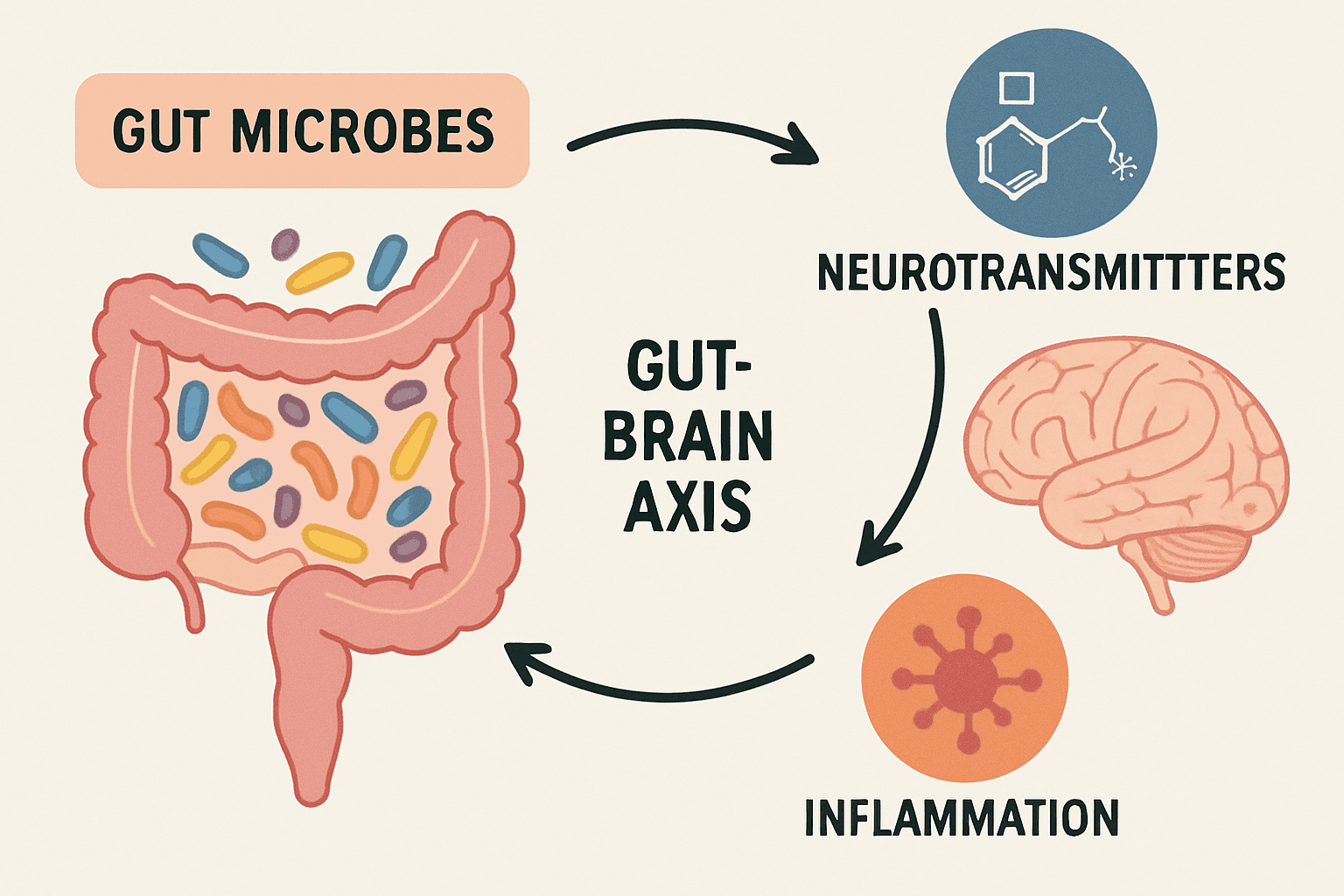
The trillions of microbes in our intestines – collectively the gut microbiome – act like an “invisible organ” that shapes digestion and brain function. Healthy gut flora produce beneficial compounds: for example, short-chain fatty acids (SCFAs) (like butyrate) from fiber fermentation, which support brain immune cells and mood regulation. Microbes also generate neurotransmitters (serotonin, GABA, dopamine) or their building blocks. As noted, most of our serotonin is made in the gut. These neurotransmitters can act on nerve endings connected to the brain (via the vagus nerve) or enter circulation to influence brain chemistry. Experiments show that transplanting gut bacteria from depressed humans into rodents can induce depression-like behaviors in the animals, underscoring that microbial changes drive mood.
Importantly, depression and anxiety have been repeatedly linked with gut dysbiosis (an imbalance of gut bacteria). A 2025 review found that people with depression or anxiety often have more inflammation-promoting microbes and fewer anti-inflammatory, SCFA-producing bacteria. For instance, depressed subjects tend to show higher levels of certain pro-inflammatory gut bacteria (Actinobacteria, Proteobacteria, etc.) and lower levels of beneficial SCFA-producers (like Ruminococcaceae, Lachnospira). This shift may drive low-grade inflammation: depressed patients often have higher blood levels of inflammatory markers and antibodies to gut-derived LPS. The good news is that interventions which restore gut balance (for example probiotics or high-fiber diets) appear to counteract inflammation and improve mood.
Dietary Patterns: Feeding the Gut for Mental Health
Decades of research link diet quality to mental health. Diets high in processed foods, sugar, unhealthy fats and low in fiber create gut dysbiosis and inflammation. A pro-inflammatory “Western” diet (rich in refined carbs, red/processed meats, saturated fat and sugar) consistently raises systemic inflammation. Such inflammation can alter neurotransmitter metabolism and activate stress hormones (the HPA axis), contributing to anxiety and depression. In contrast, eating anti-inflammatory, fiber-rich foods supports a healthy microbiome and brain. For example, the Mediterranean diet – rich in vegetables, fruits, whole grains, legumes, fish, olive oil and nuts – is associated with lower depression risk. A 2023 trial found that patients taught a Mediterranean-style eating pattern showed significant improvements in depression and anxiety scores (after adjusting for baseline) compared to controls. Nutrients common to healthy diets (such as omega-3 fatty acids from fish, B vitamins, magnesium, zinc and antioxidants from plants) have been linked to reduced depression risk.
High-fiber plant foods are especially beneficial: they feed SCFA-producing bacteria and suppress inflammatory gut bugs. Studies show that consistent consumption of fruits, vegetables and whole grains (all high in prebiotic fibers and polyphenols) correlates with better mood and lower levels of inflammatory markers. In one controlled study, a 4‑week “psychobiotic diet” enriched in prebiotic fibers and fermented foods led to a sharp drop in perceived stress (a 32% reduction) in healthy adults. Adherence to this diet (raising daily fiber intake from ~26 g to ~29 g and adding yogurt, kimchi, kefir, etc.) produced the stress drop; those less adherent saw smaller benefits. These findings suggest even moderate dietary changes – more fiber, more fermented foods, less processed junk – can tangibly lower stress.
Key point: Eating a balanced, anti-inflammatory diet fosters a healthy gut microbiome. Conversely, diets high in sugar, fat and additives disrupt gut ecology and may exacerbate anxiety and depression.
Probiotics and Prebiotics: Allies for Mood
Probiotics are live beneficial microbes (often in yogurts, kefir, sauerkraut, kimchi, miso, or supplements). When ingested in sufficient amounts, some probiotic strains can favorably alter gut flora and boost mental well-being. Multiple clinical trials (though varying in design) have tested probiotic formulas for mood. A 2024 systematic review of trials from 2014–2023 found that “the majority of the most recent literature suggests a beneficial role of probiotics in the treatment of depression and anxiety”. For example, in small human studies, certain Lactobacillus and Bifidobacterium supplements lowered anxiety scores and improved depression inventories; one trial even found women eating probiotic yogurt became noticeably calmer when stressed. Animal research adds support: in mice, giving Lactobacillus casei helped reverse depression-like behaviors and inflammation caused by antibiotics.
Prebiotics (dietary fibers that feed good gut bacteria) are also mood-promoting. Foods rich in inulin, fructooligosaccharides or resistant starch (like onions, garlic, asparagus, bananas, oats, legumes) selectively boost friendly bacteria such as Bifidobacteria. While clinical data on prebiotics alone are still emerging, they reinforce overall gut health. Importantly, high-fiber foods often contain prebiotics, so a fiber-rich diet naturally supplies them. In practice, focus on both probiotics and prebiotics together. Even simple steps – adding a daily cup of live-culture yogurt or a serving of sauerkraut, plus eating more beans, berries, and whole grains – can nurture a “psychobiotic” diet for the brain.
Lifestyle Factors: Beyond Food
Gut-brain health is not governed by diet alone. Other lifestyle habits also play a role. Regular exercise has anti-inflammatory effects and promotes a more diverse gut microbiome. Physical activity is well known to improve mood, reduce anxiety and stress, and studies suggest changes in the microbiome may contribute to these benefits (for example, exercise increases production of gut-derived butyrate and other SCFAs). Stress reduction is likewise important: chronic stress alters gut motility and barrier function, letting pro-inflammatory substances leak into the body. Practices that lower stress – such as mindfulness meditation, yoga, adequate sleep and social support – can benefit both the gut and the mind. (One trial noted that healthcare workers who practiced regular meditation had fewer depressive symptoms.) Finally, getting enough sleep helps regulate hormones and gut bacteria diversity, while avoiding smoking and excessive alcohol protects gut integrity. In summary, combining a wholesome diet with positive lifestyle habits (exercise, relaxation, sleep) creates a strong foundation for a resilient gut-brain axis.
Science-Backed Gut-Brain Diet and Lifestyle Tips
To support both gut and mental health, consider these research-informed strategies:

- Eat plenty of fiber-rich plants. Load up on vegetables, fruits, legumes, and whole grains. These contain prebiotic fibers and polyphenols that fuel beneficial gut bacteria. For example, leafy greens, broccoli, berries, apples, oats and beans are excellent choices.
- Include fermented foods daily. Yogurt with live cultures, kefir, sauerkraut, kimchi, miso or kombucha introduce natural probiotics. Even a small serving can help diversify your microbiome and has been linked to better mood and lower stress.
- Choose healthy fats and proteins. Opt for olive oil, nuts, seeds and fatty fish (salmon, sardines) instead of processed oils and red meats. Omega-3 fats in fish and nuts are anti-inflammatory and support brain cell function. Studies associate diets rich in these fats with lower depression risk.
- Limit sugar and highly processed foods. Sodas, sweets, chips and processed meats promote inflammation and harmful gut bacteria. Reducing refined sugars and artificial additives may ease anxiety and depression symptoms.
- Stay hydrated and balanced. Drinking enough water and moderate amounts of coffee or tea helps maintain healthy digestion. (Coffee and tea, in moderation, also contain polyphenols that benefit gut microbes.)
- Probiotic supplements (if needed). If you have persistent digestive issues or aren’t eating fermented foods, a clinically-tested probiotic supplement (containing strains like Lactobacillus and Bifidobacterium) may help. Look for reputable brands and discuss use with a healthcare provider. Research suggests supplements can modestly reduce anxiety/depression symptoms.
- Exercise regularly. Aim for at least 150 minutes of moderate exercise per week (brisk walking, cycling, swimming, etc.). Exercise enhances microbial diversity and mood regulation.
- Prioritize sleep and stress management. Good sleep hygiene and relaxation techniques (meditation, deep breathing, spending time in nature or with friends) reduce stress hormones that otherwise harm gut integrity.
Sample Gut-Healthy Meal Plan
Below is a sample one-day meal plan emphasizing gut-friendly, mood-supporting foods. This is illustrative; adjust portion sizes and food choices for your needs. The focus is on fiber, probiotic foods, and anti-inflammatory ingredients.

- Breakfast: Oatmeal made with milk (or plant-milk) topped with blueberries, sliced banana and a spoonful of plain yogurt (with live cultures). Sprinkle with flaxseeds or walnuts.
- Morning Snack: A small bowl of mixed berries or an apple, plus a handful of almonds.
- Lunch: Mixed greens salad (spinach, arugula, romaine) with cherry tomatoes, carrots, cucumber and chickpeas, dressed with olive oil and vinegar. Add a side of sauerkraut or pickled vegetables.
- Afternoon Snack: Carrot/celery sticks with hummus or a probiotic-rich kefir (plain or flavored with fruit).
- Dinner: Grilled salmon (or tofu) with a side of steamed broccoli and quinoa or brown rice. Drizzle with olive oil and lemon. Optionally include a cup of miso soup or yogurt.
- Dessert (optional): A few squares of dark chocolate (70% cocoa) or a probiotic yogurt with sliced fruit.
This meal plan provides whole grains, lean protein, healthy fats, ample vegetables/fruits, and fermented foods, all of which support a healthy gut microbiome. Over time, a variety of such meals (and spices like turmeric/ginger, tea, and extra veggies) can help maintain gut balance and promote better mood and stress resilience.
Conclusion
Modern science is revealing that our mental well-being is closely tied to our digestive health. The billions of bacteria in our gut influence brain chemistry through the vagus nerve, immune signals and metabolic messengers. A diet rich in fiber, plants, healthy fats and fermented foods tends to foster a resilient, anti-inflammatory microbiome – and studies consistently find that such diets are associated with lower rates of anxiety and depression. Conversely, diets high in processed foods and sugar can provoke gut inflammation and mood disturbances. While no single food is a cure for mental illness, improving gut health is a promising strategy to complement conventional therapies. As one review notes, a century of research now establishes the gut–brain axis as “a critical pathway” in mood disorders. By mindfully choosing foods and lifestyle habits that support our gut microbes (and keeping stress in check), we can help nurture both a healthy mind and a healthy microbiome.
Sources: Recent scientific reviews and clinical trials in nutrition, gastroenterology and psychiatry underpin the information above, indicating how dietary and lifestyle choices influence the gut–brain connection and mental health.






